The term high risk pregnancy often causes concern to clients. They may feel well ad healthy, and have always been. Sometimes at their first appointment in pregnancy they find that they are classified as having a “high risk” pregnancy. Sometimes some new information arises during the pregnancy and you are told that you have become high risk. Why? What does this mean?
To understand this, we need to start by recognising that life is full of risks (or chances). Every day we are exposed to risk – there is a chance of choking on your breakfast, falling downstairs and so on. Most of those risks, though possible, are not things we worry about. Other things involve greater risk. We may take action to reduce the risk, such as looking before you cross the road, wearing a seatbelt etc. Some things pose major risks which may not feel worth taking for one person, but which another would consider ok or worth taking. Think of bungie jumping or Russian roulette!
Pregnancy is a time when your body has to work very hard and many physiological processes have to adapt. This can be challenging. Sometimes things get complicated. There is no such thing as a risk-free pregnancy. In fact, when we think about it we realise that there is no such thing as risk free life. In the UK midwives are skilled and able to manage the changes and issues that comes with normal pregnancy. We term this low risk pregnancy.
Sometimes factors exist, or are identified during the pregnancy, which might fall outside the usual remit of the midwife. We talk about things being outside our “scope of practice” – that scope of practice being determined by the NMC – see last week’s blog https://yourmidwife.org.uk/blog/midwifery-in-the-uk/. In a box ticking exercise, identifying a factor which is outside the midwife’s scope of practice means that the pregnancy is then considered “high risk” or (medical) consultant led. In the NHS, each hospital develops their own guidelines which identify factors which mean that a midwife should refer a client to see a consultant. It doesn’t mean that the care of a midwife has become irrelevant- in fact it may be a whole lot more relevant – but recognises that some situations benefit from the dual perspectives and knowledge of both midwives and doctors.
The effects of being labelled as having a high risk pregnancy can be profound. Far too often I speak to people who have seen this written on their notes, or are told “this is a high risk pregnancy” but don’t really understand why. My first advice is always to ask directly what factor or factors have led to this label. You need to know what the identified risk is in order to figure out to what you feel about it. It is certainly not unknown for women to ask the question, only to find that no-one really knows. It can be super frustrating to go to an appointment with a consultant because you have the label of high risk pregnancy, only to be asked by the doctor why you are there. If it is suggested that you have extra appointments, scans or blood tests, it is totally reasonable that you ask why that is being suggested and how it might benefit you. I have also met many people who find themselves having very medically defined care in which the normal aspects of pregnancy and the huge life changes it brings can be rather overlooked.

The range of issues that can lead to this are wide and varied. In some cases it might be a factor such as your age which triggers a tick box on a particular organisation’s guidelines. For example, with one hospital team being age 40 might trigger their interest, in another unit it may not. Raised BMI (body mass index) is another such example which is very controversial and I thoroughly recommend Sara Wickham’s book https://www.sarawickham.com/plus-size-pregnancy/. Both of these are examples of situations where it is clearly nonsensical to have a simplistic high risk:low risk view. However, in a system as complex and busy as the NHS most people recognise that some rather generalised forms of decision making are expedient for the system, but may not best address the issues of a particular individual.
Some issues are specific to one part of the pregnancy or birth. For example, if you are categorised as having a high risk pregnancy because of a strong family history of multiple pregnancies, once you have had a scan which confirms a singleton pregnancy the “risk” no longer exists and your planned care can continue solely with a midwife.
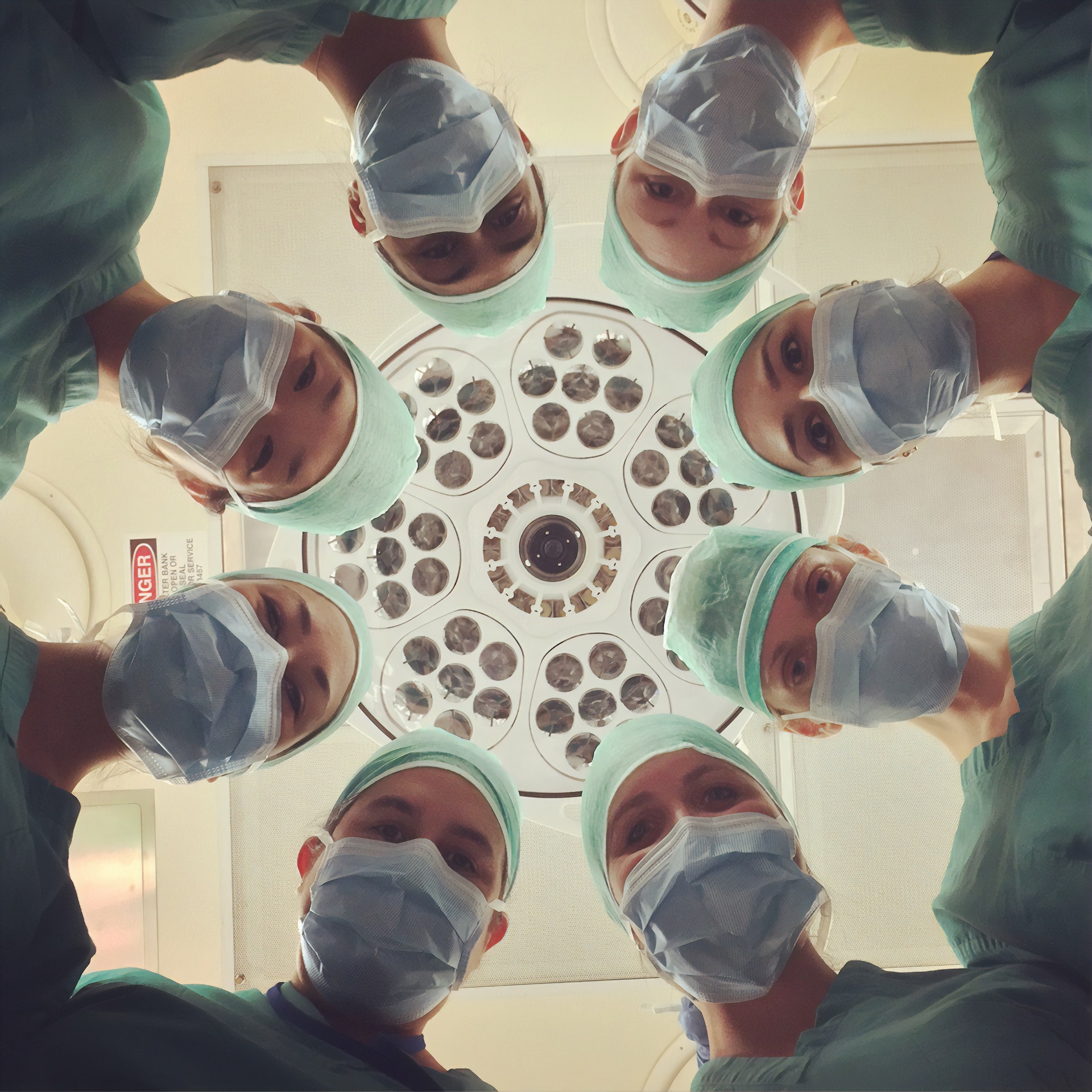
Some issues have very specific and real reasons for a multi-disciplinary approach to pregnancy, birth care and/or postnatal care. I have provided midwifery care for those with a wide range of pre-existing health issues such as diabetes, epilepsy, complex mental health conditions, previous cancer, previous organ transplants and so on. When you have a pre-existing health issue, or you there is a recurring health issue in your family, it can be very valuable to have a pre-pregnancy consultation https://yourmidwife.org.uk/blog/planning-pregnancy/. Once you are pregnant there may be a number of specialists who can be involved as we seek to provide the very best care for you and your baby.
Some high risk pregnancy gets this label because of s single factor which is poorly understood, but thought to perhaps increase the chance of things getting more complicated or not progressing as well as we would hope. A good example of this is the issue of being found to have a low PAPP-A level in the first trimester. You can read more about that here https://yourmidwife.org.uk/blog/what-causes-low-papp-a-result-in-pregnancy/.
It is important that you understand what the issue is that has led to this being labelled as a high risk pregnancy. The label rarely means that you or your baby are at serious or immediate risk of something awful happening. If it does, you would certainly be having that explained to you. It doesn’t mean that you will have to have a very medicalised pregnancy and birth (unless that is your preference). It doesn’t mean that you will “have to” be induced or have your baby in hospital. It most commonly means that there is a factor which your care providers need to be mindful of and which may affect choices you are offered.
Although people often assume that as a private midwife I mainly deal with “normal” pregnancy and birth and that my clients almost always choose homebirths, that actually isn’t the case. Midwifery is a very broad profession and many of us have special interests. Whilst I love “normal” and homebirth can be wonderful, I have special interest in working with people who have complicated pregnancies, and I am very comfortable working as part of a multi-disciplinary team and often also support those giving birth in hospital.
If you have been told that you have a high risk pregnancy and you are worried about what this means – ASK! Whether this is said at a booking appointment, or later in pregnancy, ask what has led to the label, what the implications might be and what the additional care and management options might be. That allows you to size up the risk and to be actively involved in deciding what (if anything) to do about it. I continue to offer single appointments if you would like to talk through any issues about your choices and experiences. An hour or two in the comfort of your home is often a better way to learn about, ask questions and think through information.